The Top Three Challenges in Denial Management
Regardless of the industry or profession, everyone wants at a minimum to be compensated fairly for the services they provide.
Healthcare providers are no different, yet as we covered in Reverse Engineering Denials Management, 65% of claim denials are never worked, even though ~69% of all these denials are appealable. As denials have grown to 18%-20% of claims submitted, these organizations are clearly losing untold amounts of money that they have rightfully earned. So why are many of them not acting?
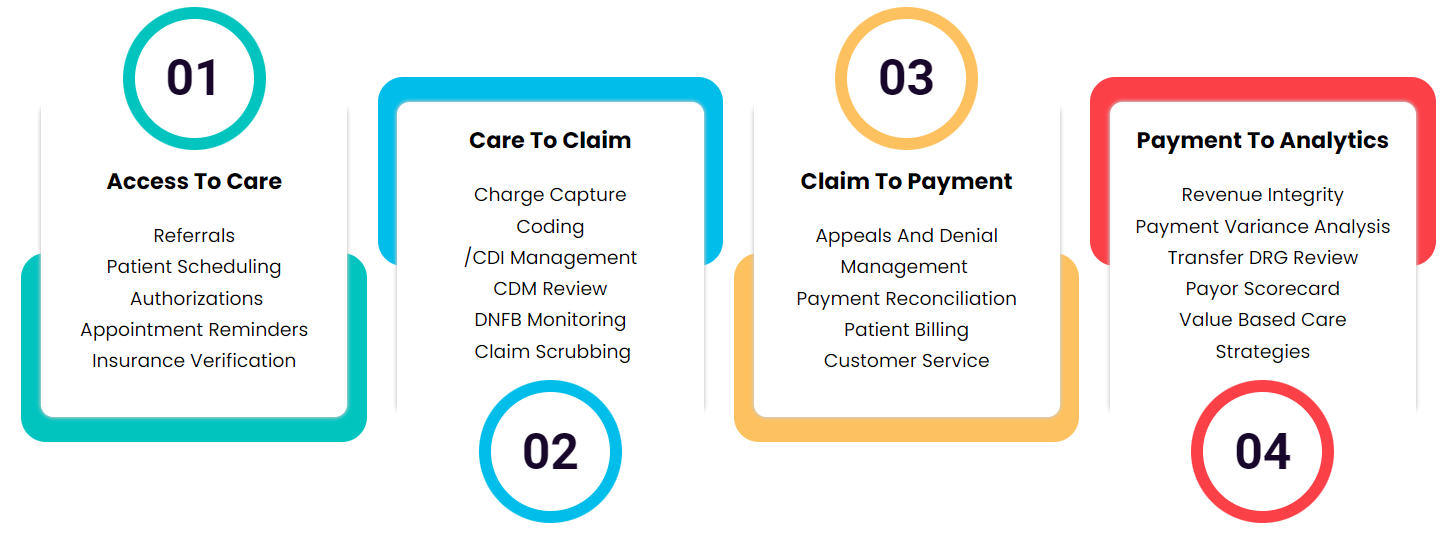
Denials management requires investigating every denial down to its root cause and extrapolating denial trends across insurance carriers and the industry in general. This information is then used to redesign the entire process to reduce future claim denials.
Which is to say, denial management is not easy. It’s s a multi-layered process that presents many obstacles to organizations that are looking to reduce their denial rates. But as always, understanding the challenges you’re up against is the first step to overcoming them.
The first step is to identify just how big an issue denials management is for your organization.
According to the American Academy of Family Physicians (AAFP), add the total dollar amount of claims denied by payers within a given period and divide by the total dollar amount of claims submitted.If possible, your rate should also be segmented by payer, provider, and reason for denial.
Once you have this baseline for your specific organization, you can prepare yourself to address your most pressing challenges of denial management. While every organization will have their own unique obstacles, the following are among the top three for the majority of our partners.
Lack of Staff Appropriately Trained in Denial Management
Some of the first mistakes in denial management occur at the registration desk. In fact, 30% to 40% of denied claims result from registration and pre-service-related challenges. Staff members in many organizations are busy doing a multitude of administrative tasks, required to fill many different roles, and must deal with the ever changing industry and regulatory requirements.
While there are a number of resources for denial management staff training, such as this training course by AAPC, many staff members may not have the time to complete them during working hours and would be resistant to doing so on their own time. Regardless, it is not a given that these types of materials would prepare staff to effectively solve the denials challenges unique to the specific organization. Considering the prevalence of turnover in these roles, even the most effective staff training may not yield sustainable results.
Lack of Automation
A survey from the Healthcare Information and Management Systems Society (HIMSS) found that about one-third of providers continue to perform their denial management process manually. For hospitals and health systems, only 38% currently apply automation to denials management, despite 78% applying automation to other areas of revenue cycle management.
Such manual processes leave too much room for human error, offer less transparency, are usually extremely time-consuming, and increase the turnaround for claims, leading to severe backlogs and losses of revenue.
Lack of Financial Resources
Regardless of the reason, incorrect coding can not only cause valid claims to be under-compensated, delayed, or rejected and denied, they can also cause a backlog of paperwork for your staff that can lead to greater errors going forward. To that end, repeat errors in coding over time, particularly for upcoding, can result in penalties under the False Claims Act.
By not investing in a denial management solution that enables them to correctly submit claims initially, an organization might not be able to recoup enough revenue to address correcting and appealing denied claims.
Similarly, without technology to effectively prioritize, manage, and channel claims, organizations are unlikely to be able to streamline their denial management and obtain the revenue patients and payers owe them.
In fact, only 17.3% of the organizations who responded to the HIMSS survey mentioned above had resources specifically focused on front-end denial prevention tasks. When you compare this to the fact that 67% of the denials originate from front end workflows, you can see why organizations are losing the game when it comes to denial management.
Overcome Your Denial Management Challenges
In a previous article, we explored the Top Five Reasons Claims Are Denied, which includes patient eligibility, missing or incorrect data, duplicate or late submissions, improper or outdated CPT/ICD-10 Codes, and missing/incomplete prior authorization.
It’s no small wonder that the three main challenges in denial management we covered today’s lack of specialized training, lack of automation, and lack of financial resources all cause or contribute to the same reasons claims are denied again and again.
Unfortunately, most organizations today are working with resources that are limited on a variety of fronts. This leads many to try DIY solutions that do not solve the root causes of denials. While we at Medical Practice Success understand why these same resource crunches can dissuade organizations from outsourcing, we believe that if an organization focuses on the real goal of increasing medical group revenue the optics change to ROI.
In that light, working with a group like MPS to drive incremental revenue increases, improve overall profitability, and maximize reimbursement can be a cost effective path to overcoming a variety of revenue cycle challenges, not only in denial management.
Reach out to Medical Practice Success today to overcome your denial management challenges. Our partners typically see a 5% to 10% growth in revenue with our revenue cycle management (RCM) services. If you want to protect and improve your organization’s financial future, get started with MPS today.

